
Osteochondrosis of the lumbar spine is a pathology of the musculoskeletal system, which is accompanied by degenerative-dystrophic changes in bone tissue and dysfunction of the five lower vertebrae (from 20 to 24). The disease causes discomfort to the patient and is characterized by specific symptoms – pain, stiffness of movement. Osteochondrosis of the lower back occurs in waves with periods of exacerbations and remissions. According to statistics, this form is one of the most common. Uncontrolled pathology often leads to irreversible changes and a significant deterioration in quality of life. However, with a competent integrated approach, osteochondrosis can be successfully treated.
Main causes of pathology
There are no precise data on why degenerative-dystrophic changes in the spine are triggered. It is believed that the trigger for the development of pathology is premature age-related changes in the joints. They can be genetic - transmitted through heredity, but most often they initially manifest themselves under the influence of unfavorable factors.
The main cause is considered to be incorrect load distribution on the spine. Osteochondrosis of the lumbosacral spine can develop with:
- wearing high-heeled shoes;
- carry a bag or backpack alternately on one shoulder;
- sleeping or resting in an uncomfortable position for long periods of time;
- sedentary activity;
- Lift weights.
The risk groups for the development of osteochondrosis include the elderly, characterized by natural destructive changes in cartilage and bone tissue, professional athletes who train daily and intensively, pregnant women, whose center of gravity shifts with the growth of the fetus and the load on the abdomenThe back is noticeably increasing, office workers are forced to spend a lot of time sitting.
In addition to external risk factors, doctors also name a group of internal ones. This includes:
- previous musculoskeletal injuries;
- curvature of the spine;
- flat feet;
- congenital dislocation or subluxation of the hip joint;
- autoimmune diseases;
- inflammation of joint tissue;
- pathologies of the circulatory system;
- endocrine diseases;
- Obesity.
Osteochondrosis of the lower back can also be caused by intoxication and prolonged dehydration, bad habits, calcium deficiency and mechanical impact on the lower back - bruises, blows, falls.
Osteochondrosis of the lumbar spine: symptoms
The pathology affects not only the bone tissue itself, but also the entire moving segment of the spine - vertebrae, intervertebral discs, ligaments, surrounding soft tissues, blood vessels and nerve endings. Osteochondrosis of the lumbar spine develops gradually and slowly, the symptoms of which become clear when there is significant damage. In the early stages there is moderate discomfort when exerted, in the later stages it is acute, unbearable pain. The clinical symptoms are pronounced in the acute stage. They subside during the remission phase, and in the early stages this also happens without treatment.
Osteochondrosis of the lumbar spine - symptoms:
- pain in the affected area of the spine;
- Radiation of pain upwards into the area of the shoulder blades or downwards into the pelvic and hip joints;
- persistent feeling of tension in the lower back;
- difficulty bending and turning the body;
- lounging;
- lameness;
- muscle weakness or, conversely, increased tone;
- Tingle.
Not all of the symptoms described are always present at the same time. Pain may be associated with limited mobility, but not with muscle weakness or numbness. Any of the above signs is a reason to see a doctor.

Stages of the disease
The intensity of symptoms associated with osteochondrosis of the lumbosacral spine directly depends on the degree of development of the pathology. There are four of them in total.
- First stage. The first structural and functional changes begin. Intervertebral discs dry out and can crack. Symptoms at this stage are mild. Many patients confuse it with fatigue after a day at work, wearing uncomfortable shoes or playing sports. The main signs of early osteochondrosis are mild discomfort in the lower back, which increases when bending and twisting. Mild pain is possible, which goes away on its own after rest.
- Second stage. The height of the intervertebral discs decreases and the bone structures move closer together. This leads to a new set of symptoms – stiffness and pain. The pain becomes longer and more intense and can radiate into the pelvis and legs.
- Third stage. At this stage the vertebrae become deformed. Protrusions form - intervertebral discs bulge into the area of the spinal canal, but the fibrous rings remain intact. The main symptoms are severe pain that is bothersome even at rest, reduced sensitivity, grinding and clicking when moving, tingling and numbness in the lower back.
- Fourth stage. Pathological changes continue to progress. The functions of the vertebrae are lost. Hernias form. Osteophytes – bone growths – form. Blood vessels can become pinched and nerve fibers can become pinched. Against the background of deteriorating blood circulation, dysfunction of the pelvic organs occurs. In men, the risk of erectile dysfunction increases; in women, disruptions in the menstrual cycle are observed. Advanced osteochondrosis is manifested by severe lumbago in the lower back, lameness, limited mobility up to complete immobility and increased temperature.
If you are worried about lumbar osteochondrosis, treatment directly depends on the stage at which the disease is diagnosed. In the early stages, the doctor has many other recovery methods and techniques in his arsenal. Detection of degenerative-dystrophic changes in the initial stages allows conservative treatment of the pathology without resorting to surgical intervention.
Forms of pathology
The division into forms is based on the characteristics of the pain syndrome, which is always accompanied by osteochondrosis of the lumbar-sacral spine. There are three in total:
- Lumbago. This is an acute stabbing pain that makes movement impossible. Causes of pain can be pinched nerves or muscle spasms.
- Lumbodynia. This is a long-lasting, aching pain. It is characteristic of the stage of formation of protrusions and hernias. A sprain of the ligaments can also cause discomfort.
- Sciatica. This is severe pain that radiates into the pelvic area. The patient complains of pain when walking, sitting or changing posture.
Depending on the accompanying symptoms, two other forms of pathology are distinguished. The patient can be diagnosed with:
- Radiculopathy. Accompanied by compression of nerve endings due to deformation of the vertebrae. In this form of the disease, sensitivity decreases and the affected area becomes numb. Pain and tingling are expressed. Possible decrease in muscle tone, impaired reflexes, tingling in the legs.
- Discogenic lumbar osteochondrosis. This is a serious disease in which the patient's movement is restricted. His lower back and limbs are numb. Other symptoms include general weakness, fever, involuntary urination and, if the illness lasts for a long time, weight loss.

Risk of spinal disease
If left untreated, osteochondrosis is fraught not only with unbearable pain and stiffness of movements, but also with a number of pathologies that can develop against its background. The most common complications:
- intervertebral hernia;
- Inflammation of the sciatic nerve;
- radiculitis;
- Paresis.
In order to prevent concomitant diseases, treatment of osteochondrosis must be started immediately after its discovery. With a competent therapeutic approach, it is possible to stop or significantly slow down the destruction of bone and cartilage tissue.
Methods for diagnosing pathology
Osteochondrosis of the lumbar spine must be differentiated from other pathologies of the musculoskeletal system that can occur with similar symptoms. The first stage is a consultation with a neurologist, orthopedist or surgeon. The doctor clarifies complaints, collects an anamnesis, conducts a physical examination, paying attention to the peculiarities of the patient's posture and posture, the nature of his work activity, bad habits and concomitant diseases.
For the most accurate diagnosis, instrumental techniques are used:
- MRI;
- radiography;
- myelography with contrast medium;
- Multi-slice CT.
Each of the diagnostic procedures allows the doctor to assess the current condition of the lumbar and sacral spine. The images clearly show structural changes in the vertebrae, which indicate the stage of osteochondrosis. Based on the data obtained, the specialist decides on the tactics for further treatment of the patient.
Laboratory diagnosis is not crucial, but tests may be recommended if necessary. In particular, when lumbar osteochondrosis is diagnosed, treatment may be prescribed based on the results of blood tests. They are necessary to clarify the intensity of inflammatory processes in the muscle fibers adjacent to the spine.
Lumbar osteochondrosis: treatment
The fight against pathology occurs under the supervision of a neurologist and begins after a comprehensive diagnosis, during which the degree and extent of tissue damage are determined. Modern medicine offers a number of effective conservative methods. If their use does not lead to the expected result, doctors resort to surgery.
Lumbar osteochondrosis: treatment with physiotherapeutic methods
All physiotherapeutic techniques are good because they have a comprehensive effect on the sacral and lumbar spine. This approach allows you to manage pain, reduce inflammation and restore normal blood circulation.
If osteochondrosis of the lumbar spine progresses, treatment should be comprehensive. Patients with complaints are prescribed:
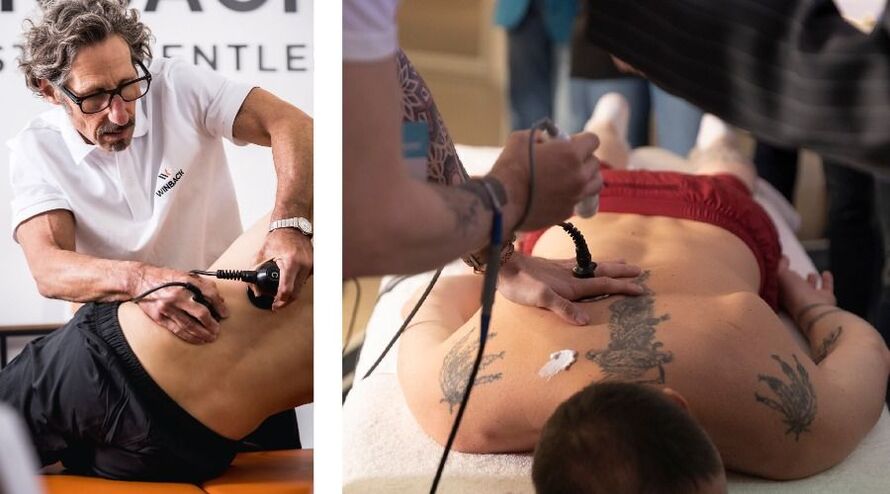
- Electrophoresis – exposure to constant electrical impulses on the problem area with the possibility of using medications for external use;
- diadynamic therapy – a variant of electrotherapy with pulsed currents;
- Magnetotherapy – treatment with alternating or static magnetic fields;
- Ultrasound therapy – the influence of high-frequency sound waves;
- Shock wave therapy – exposure to low-frequency acoustic impulses;
It is important to take into account two nuances. Firstly, the effect of physiotherapeutic treatment becomes noticeable only after a series of procedures, the duration of which is selected individually for each patient. Secondly, physiotherapy works as an independent method for first degree osteochondrosis. For large lesions, it is recommended as an auxiliary technique in addition to medical and surgical treatment.
Lumbar osteochondrosis: treatment with medication
Pharmacotherapy for lesions of the lumbar and sacral spine is aimed at relieving acute pain and suppressing inflammatory processes. The method is relevant in the acute stage, when symptoms interfere with a full life.
How lumbar osteochondrosis is treated with medication is always decided individually. A neurologist can prescribe drugs from different pharmacological groups. Basic:
- NSAIDs (systemic and local) to suppress inflammation in the vertebrae and adjacent tissues;
- muscle relaxants to relieve muscle spasms;
- angioprotectors to improve blood circulation;
- Chondroprotectors to protect the cartilage tissue of the intervertebral discs from destruction;
- B vitamins to improve nerve conduction;
- Analgesics for stabbing pain that limits mobility.
Exercise therapy as a method of treating pathologies in the sacral and lumbar regions
Intensive training for osteochondrosis is strictly prohibited, but you cannot completely do without physical activity. On the contrary, exercises of moderate strength and duration help restore blood circulation and relieve pain.
How to treat osteochondrosis of the lumbar spine with exercise therapy:
- Train with a trainer. The trainer shows you which exercises are permitted in the respective situation and ensures that they are carried out correctly. Even the smallest technical defects can significantly impair the effectiveness of the training or even cause damage.
- Prepare carefully for the lesson. Before training, it is recommended to warm up the muscles - you can gently massage the lower back and sacrum.
- Strictly dose the load. The lower back is a vulnerable area. To avoid overexertion, you need to monitor the duration of classes. Their optimal duration is no more than 20 minutes.
- Increase exercise intensity gradually. Simple exercises and short programs are suitable for beginners without experience. For those who have been doing exercise therapy for a while, you can move on to more complex options.
- Remember to be regular. A one-time training does not bring any visible improvements. Pain in the lumbar and sacral spine decreases if the patient practices exercise therapy regularly - ideally twice a week.
- Consider contraindications. Physiotherapy has been proven to be a safe method of treating osteochondrosis, but there are limitations. You should stop exercising if you feel unwell: fever, weakness, or rising temperature.
Lumbar osteochondrosis, the treatment of which should take into account the period of illness, will not bother you if all the rules are strictly followed.
- In the acute phase. Only gentle and slow movements are allowed. If pain increases during exercise, you need to take a break and give your joints a rest.
- In the subacute phase. The pain syndrome subsides, mobility is restored, which allows you to slightly increase the intensity of training and increase the duration of training. However, to avoid deterioration, you need to carefully monitor your well-being.
- In remission. For diseases of the lumbar spine, we allow the entire range of exercises, but it is important to remember that overexertion is associated with a re-exacerbation of the disease.
If lumbar osteochondrosis is diagnosed with mild or moderate severity, treatment with physical education can also be carried out at home. After the exercise technique has been perfected under the supervision of a trainer, it is not forbidden to repeat the exercises at home. For training you need an exercise mat, a roller and a ball.
Modern exercise therapy and rehabilitation rooms are equipped not only with traditional accessories, but also with special medical simulators. They help you recover gently and safely from illness and make activities more fun and interactive. For example, the neuromuscular rehabilitation system turns a rehabilitation session into an exciting competition with oneself. The patient stands on a moving platform and performs the exercises shown on the screen. Another important advantage of the simulator is the ability to track even the smallest progress in the patient's condition. The system evaluates the result of each exercise performed and the doctor can track the progress from training to training. Knowing about their own success also motivates patients to try harder and not give up.

Manual therapy
Good results can be achieved if you complement exercise therapy and medications for lumbar pathology with manual therapy. The method allows:
- eliminate hypertonicity of muscle fibers;
- relieve pain;
- Restoration of blood supply in the lumbar and sacral areas;
- improve the course of metabolic processes.
Manual therapy is an effective way to properly redistribute the load on the spine and protect against further destructive changes. The good thing about this method is that it not only relieves pain, but also prevents neurological disorders that often develop against the background of lumbar osteochondrosis.
Currently, chiropractors combine massage and physiotherapy methods, such as Tekartherapy. Electromagnetic waves penetrate deep into the bone tissue and allow you to relieve attacks of pain and quickly restore mobility.
Surgical methods
Osteochondrosis of the lumbar spine, the treatment of which is not always effective with medications, physiotherapy and exercise therapy, significantly complicates the patient's life. In some cases, only surgical intervention is useful to eliminate the pain and restore mobility to the back. Modern methods and technological equipment make it possible to carry out minimally invasive operations with a shortened rehabilitation period.
The following intervention methods are relevant for osteochondrosis:
- endoscopic removal of intervertebral hernias – using microsurgical instruments and a built-in camera;
- transfacet removal of intervertebral hernias – with neurosurgical tube dilators;
- Laminectomy – surgical removal of pathologically changed bone processes;
- Microdiscectomy – elimination of the hernia bulge.
Direct indications for surgical intervention are recurrent hernias, spinal stenosis, when the spinal canal narrows, and degenerative spondylolisthesis, a pathology in which the vertebrae are displaced relative to each other. In all other cases, with confirmed osteochondrosis of the lumbar spine, doctors try to carry out treatment using conservative methods.
Disease prevention
Symptoms of osteochondrosis cause inconvenience and treatment of the pathology can take a long time. It is much more effective to protect the sensitive lumbar spine from overload in advance. For prevention it is recommended:
- Organize your workplace properly while working in the office. The back of the chair should support the lower back and the table should be height appropriate.
- Avoid uncomfortable shoes. The optimal heel height for women is up to 5 cm. In addition, it is advisable to exclude flat soles as they contribute to foot deformation and flat feet - one of the factors
- Risk of osteochondrosis.
- Exercise. Lifting heavy objects should be avoided. Swimming, walking and cardio training are useful if there are no contraindications.
- Eat a balanced diet. The diet must include foods containing calcium, phosphorus and B vitamins. These are fish, dairy products, leafy vegetables and grains. These substances are needed to strengthen all joint elements and to support the nervous system.
- Make sure you get enough sleep. It is better to sleep on an orthopedic mattress of medium firmness. It ensures an anatomically correct posture in which the body rests from everyday stress.
- Control body weight. Obesity is one of the provoking factors. With a normal weight, the load on the spine is sufficiently distributed and the risk of circulatory problems is minimized.
The prognosis for patients with osteochondrosis directly depends on the degree of damage to the vertebrae. That's why a timely diagnosis is extremely important. If you are worried about lower back pain and the images reveal destructive processes in the initial stages, you need to start treatment. In the early stages, medication and physiotherapy are effective. In later cases, it is rarely possible to forego surgery. As an additional supportive measure, exercise therapy can be used in any form and at any stage.
































